Hall ticket no 1801006113, A case of 60 year old male, with cheif complaints of Hematuria.
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment.
A 60 year old male, resident of appalgudathanda suryapet district, came to opd with chief complaints of blood in urine, since 2 months.
C/c: blood in urine since 2 months
History of presenting illness:
Patient was apparently asymptomatic 2 months back. Then he noticed blood in urine, which insidious in onset, gradually progressive. Increased in frequency of urine, mainly during night times for every 20 min(40-50ml).
Urine is red in colour. Incontinuity of urine is present, at first patient passes red colour urine and the urine stops for 2 seconds later he passes black coloured clots with burning sensation.
H/O shaking hands since 1 year
No H/O fever, cough and cold.
No H/o orthopnea and paroxysmal nocturnal dyspnea.
No H/O nausea, vomiting, loose stools and constipation.
No H/O abdominal distension, abdominal pain.
Past history:
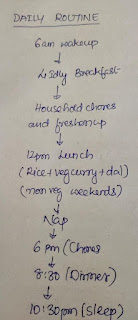
Daily routine-
History of hydrocele, since 15 years.
He worked as an driver in Priya factory, as lorry, ambulance and tractor driver in the same factory, worked there for 20 years.
History of trauma 15 years back, while lifting the lorry back door, slipped and got hit during this.
After this incindent in 1-2 months he noticed a swelling in the groin which is gradually increased in size, painless. He neglected the swelling due to no pain.
In 2019, just before corona period his wife got a swelling in the post auricular region for which he came to our hospital. Then he also went for checkup for the swelling in scrotum where our doctors diagnosed it as hydrocele. And suggested to have surgery to be done for it. But he refused to it because he has no money for surgery at that time and just his wife got treated.
In 2019 itself during corona time, he again visited our hospital with sufficient money( given by his son). But it was very difficult to do surgery at that time because of high wave period of corona patients in the hospital. Then he went back to his village.
He has 3 daughters and one son, all are married and lives at different places except his son who lives in the same village.
His first daughter was died by committing suicide of family issues and disturbances with her husband. Then the patient(father) filed a case against the husband and their family. After this incident the son in law filed a case against the patient itself that they tried to ruin their family in several ways.
A case was filed against this patient and then due to this the factory management removed him from his job 15 years ago.
From then he was staying at home with no specific job, but went to some contracted works in farming fields.
No H/O HTN, diabetes, asthma, epilepsy, TB.
No H/O any past surgery.
H/O fracture of left humerus at distal end, when he was 20 years old, while cutting a tree. Then he got treated for it with reduction and plaster of Paris. But the treatment resulted in malunion.
PERSONAL HISTORY:
Diet: mixed
Breakfast: 4 idly/ 3dosas with chutney / 3 bonda with chutney
Lunch: 1 cup rice with vegetable curry( tomato, brinjal, dal, potato etc)
Dinner: 1 cup rice with vegetable curry and curd rice.
Consumes meat every Sunday, 4 times per month.
Daily intake in calories(avg):
Idly(1)- 135 cal
Chutney - 331 cal
Rice - 206 cal
Vegetable curry- 85 cal
Curd- 118 cal
On avg total intake is 1571 cal
Deficient: 428
Appetite: normal
Sleep: adequate
Bowel and bladder: regular
Addictions: alcohol intake every 2 days 90ml, from 38 years, stopped from 2 months.
Smoking daily 10 beedi(2 days 1 packet) from 38 years, stopped from 2 months.
FAMILY HISTORY:
No significant history.
GENERAL EXAMINATION:
Patient is conscious, coherent, and co-operative. Well oriented to time place and person.
He is moderately built and moderately nourished.
Pallor- present
Icterus- absent
Cyanosis- absent
Clubbing- absent
No lymphadenopathy
No edema
VITALS:
Temperature- afebrile
Blood pressure- 120/80mm hg
Pulse rate- 96bpm
Respiratory rate- 20cpm
SYSTEMIC EXAMINATION:
Per abdomen:
On inspection
Shape of abdomen: scaphoid
Umbilicus: inverted
Movements of abdominal wall with respiration
Scars present( due to beliefs that it helps in digestion, done in childhood)
Swelling in scrotum.(hydrocele?)
No visible peristalsis, pulsations, sinuses, engorged veins.
On palpation
No local rise of temperature
Inspectors findings are confirmed
Soft and non tender
No palpable masses
Liver is not palpable
Spleen is not palpable
On percussion:
Resonance note heard
On auscultation:
bowels sounds heard
CVS examination:
Inspection
No raised JVP
No dilated veins, scars or sinuses are seen
Palpation:
Apex beat is felt in the fifth intercoastal space, 1cm medial to the midclavicular line
Auscultation:
S1 S2 heard, no murmurs
Respiratory examination:
Shape of chest is elliptical, bilaterally symmetrical
B/L airway entry positive
Normal vesicular breath sounds
Trachea appears to be central.
CNS Examination:
Conscious
Normal speech.
Higher mental functions normal
Cranial nerves intact
Motor and sensory system also normal
No neurological deficit found.
PROVISIONAL DIAGNOSIS:
Anemia under evaluation
Hematuria?
Nutritional?
INVESTIGATIONS:
12 June 2023
Complete Blood picture:



















Comments
Post a Comment